An overview of our ENT services
In these toggles, we provide some general information about the procedure we perform and the conditions we treat. For specific information about how we can help you, contact us for a consultation.
List of ENT services
- Endoscopic sinus surgery/FESS
- Septal and turbinate surgery
- Rhinoplasty/Nose job
- Mastoidectomy/Tholesteatoma surgery
- Balance and Tinnitus management
- Throat disease
- Grommets
- Tonsillectomy

Our facial surgeries give you the confidence to become
the version of yourself you most want to be
Take the first step and get a video consultation where you’ll meet expert facial surgeon, Mr Mrinal Supriya,
who will help you discover which treatment will give you the wonderful natural results you desire.
About ENT services
NHS – Functional Endoscopic Sinus Surgery
Provides an entire overview of the procedure. Click here for more information.
NHS – Tympanoplasty
Great advice for potential patients who are considering ear drum repair. Click here for more information.
NHS – Insertion of grommets
Goes over the risks, as well as the overall process of receiving ear grommets. Click here for more information.
NHS – Mastoidectomy
An NHS guide and overview of the treatment. Click here for more information.
Tinnitus.org – Balance and tinnitus
An overview of both the symptoms and treatments possible for balance and tinnitus. Click here for more information.
Cancer.gov – Parathyroid Cancer Treatment
A government website that gives a great amount of information on the cancer and treatment. Click here for more information.
NHS – Tonsillectomy
An overview of the symptoms and treatment. Click here for more information.
Consultation
We offer a free initial phone consultation with our specialist team. For the next step, we invite you to an in-person or online consultation with Mr Supriya. Consultations are £100 with Mr Supriya and are deductible from any booked surgery. This fee includes follow-up consultations.
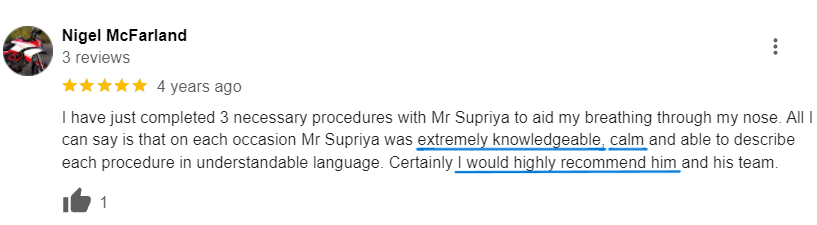
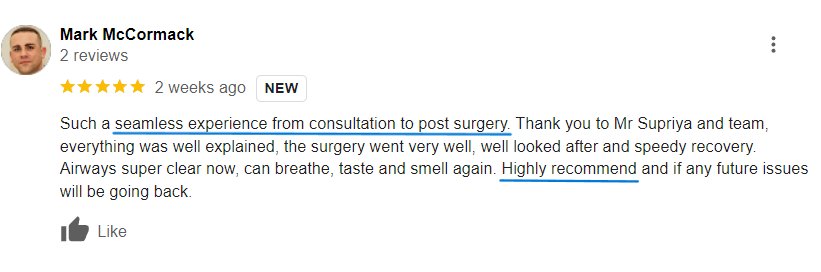
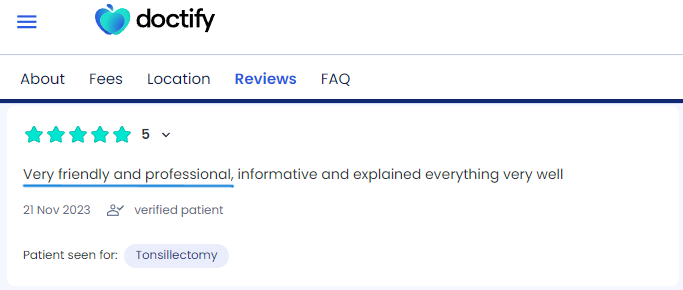
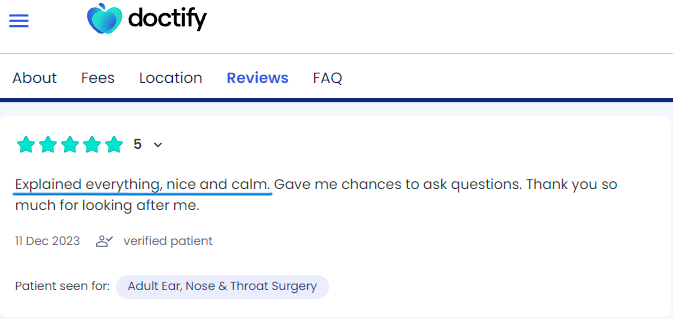
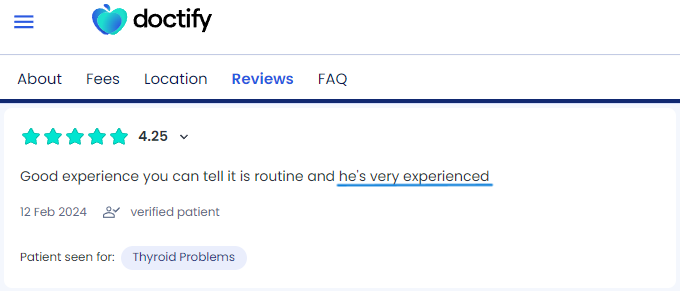
Patient Stories
It’s embarrassing looking tired at work, and social events aren’t so fun when your confidence and self-esteem are lacking. You’ve neglected yourself and feel inadequate compared to all the beautiful people around you. You deserve some self-love.
Take your first step and step into a more beautiful you!
Meet Mr Supriya - The Best
Choice for ENT Services

Meet Mr Mrinal Supriya | Facial Cosmetic Surgeon
FRCS (OTOL-HNS), MRCS Ed,
DO-HNS, MS in ENT, MBBS
Mr Mrinal Supriya is the Divisional Director of Surgery. He is highly experienced Head and Neck Surgeon, specialising in facial cosmetic surgery. He is Chief of Surgery Division (2024) and was the Clinical Director for head and neck surgery at Northampton General Hospital.
He leads complex ENT and head and neck services, including facial aesthetics & reconstruction and robotic surgery. Mr Supriya trained globally, including in the UK, Australia and the USA and worked with renowned experts like Dr Andrew Jacono. He is certified by The Royal College of Surgeons to provide facial cosmetic surgery in the UK.
Why Choose British Face Clinic for
Your ENT Services?
- Focus on natural-looking outcomes and high patient satisfaction
- Benefit from Mr Supriya’s international experience
- Advanced surgical services led by Mr Supriya at a prominent NHS hospital
- Expertise in training Oxford Deanery Trainee Surgeons
- Address both cosmetic and medical issues with comprehensive care
- Exceptionally low revision rates
- Best possible support before, during and after surgery with dedicated team access
How to schedule a consultation
To schedule a consultation to discuss ENT services, you can either call us on 07590817036, book online via our website, schedule a video consultation or visit us at one of our clinics in London, Milton Keynes, or Northampton.
What to Expect During
Your Consultation
Welcome Message from Nidhi,
Director at British Face Clinic
During your full medical consultation, we’ll discuss:
- Your surgical goals
- Medical conditions, drug allergies and medical treatments
- Current medications, vitamins, supplements, alcohol, tobacco and drug use
- Previous surgeries
Our surgeon will:
- Evaluate your general health and risk factors
- Take photographs
- Discuss your surgical options
- Recommend a treatment course
- Discuss likely outcomes and potential complications
- Preview your surgical outcome with Crisalix 3D technology (for selected procedures)
- Discuss the surgery cost and payment options
Accessible Payment
Plans Now Available
We make your procedure more accessible by offering flexible payment plans with 0% interest for the first 12 months!
It takes less than a minute to fill in the form and receive a response. ENT Services have never been so accessible!
0% financing available

Change Your Life Today
The rejuvenate face of your dreams is just a free phone consultation away.
You can get the youthful and confident look you always desired.
Our Locations
- London City
The Wellington Hospital, 15 – 17 Lodge Road
London NW8 7JA
- London City
98 Harley Street
London, W1G 7HZ
- Milton Keynes
Athena Surgical Centre
16 Davy Avenue, Knowlhill
Milton Keynes, MK5 8PL
- Northampton
The Three Shires Hospital
The Avenue
Northampton. NN1 5DR
London City
The Wellington Hospital
15 – 17 Lodge Road
London NW8 7JA
London City
98 Harley Street
London, W1G 7HZ
Milton Keynes
Athena Surgical Centre
16 Davy Avenue, Knowlhill
Milton Keynes, MK5 8PL
Northampton
The Three Shires Hospital
The Avenue
Northampton. NN1 5DR