About Snoring Treatment
In the information below we’ve provided some general information about the treatment for snoring. For specific information about how we can help you, contact us for a consultation.
What causes snoring?
Snoring is the sound generated by the vibration of the structures at the back of your throat. Mild snoring is not associated with excessive daytime sleepiness or difficulty sleeping at night. Obstructive sleep apnoea (OSA) is a condition where your breathing stops for short spells when you are asleep. However, it is not uncommon for breathing to stop for a few seconds in healthy people during sleep. Only when apnoea occurs more than five times every hour, each time for more than 10 seconds, that it becomes a health problem and we call it OSA. During these episodes, there is at least 3% to 4% fall in your blood oxygen. You wake up briefly after each episode of stopped breathing to start breathing again. You do not usually remember the times you briefly wake up, but you have a disturbed night’s sleep. This is associated with excessive daytime sleepiness, waking with gasping, choking, or breath-holding. Snoring between these episodes is a frequent complaint of bed partners and is often the reason that prompts patients to seek medical attention. 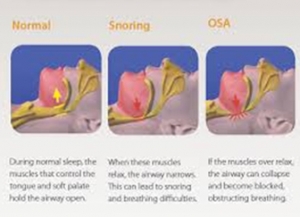
- Mild OSA – between 5-14 episodes an hour
- Moderate OSA – between 15-30 episodes an hour
- Severe OSA – more than 30 episodes an hour
Studies in the western world show that snoring affects at least 40% of men and 20% of women whereas OSA is seen in 5% of men and 3% of women. Snoring or OSA can occur at any age, including in children. However, whereas snoring is very common, few of us have OSA. Remember, very few people who snore have OSA while almost all OSA patients snore. Factors that increase the risk of developing OSA, or can make it worse, include:
- Overweight (BMI above 25) or obesity (BMI above 30)
- Thick neck (usually if the Collar size is more than 17 inches in males or 16 inches in females) because the extra tissue in the neck can squash the airway.
- Drinking alcohol before you sleep causes excessive relaxation of your muscles and makes the brain less responsive to an apnoea episode. This may lead to more severe apnoea episodes in people who may otherwise have mild OSA.
- Enlarged tonsils and adenoids
- This is the commonest cause in children
- Taking sleeping tablets or tranquilizer
- Sleeping on your back rather than on your front or side
- Having a small jaw or a jaw that is set back further than normal
- Smoking by causing an inflamed swollen airway
What symptoms could indicate OSA?
Even if you have OSA, you may not be aware of it as you will not usually remember the waking times at night. It is often your sleeping partner (or the parent if it is a child) that is concerned about the loud snoring and the recurring episodes of apnoea that they have noticed. However, you may be aware of the following problems:
- Daytime sleepiness and being tired
- Poor concentration and mental functioning
- Not feeling refreshed on waking
- Morning headaches
- Being irritable during the day
- Pass urine frequently during the night
- Night sweats
- Reduced sex drive
Are there serious repercussions of OSA?
In children, significant OSA has been linked to poor performance in studies and sports, and some studies have shown a weak link to reduced overall intellectual development. OSA can be a serious health problem in adults as studies have shown that OSA without treatment can either lead to or worsen the following medical conditions:
- Hypertension
- Heart attacks
- Stroke
- Type 2 diabetes mellitus
How do you diagnose OSA?
OSA is diagnosed based on your complaints, the findings on your physical examination, and results of tests.
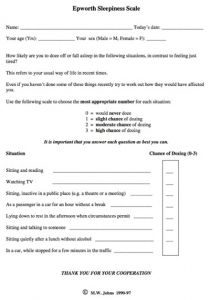
Your symptoms
If you have daytime tiredness, sometimes a questionnaire is used to measure to estimate the level of sleepiness that you feel during the daytime. A score above 10 indicates that you may have a sleeping disorder such as OSA. However, it is important to remember that many people with a high score will not have sleep apnoea, and not everyone with sleep apnoea will have a high score. Therefore, it is vital that you do not consider the score on ESS as confirmatory as this has to be reaffirmed with your complete medical assessment and other investigations.
Tests to confirm OSA
If you have any of the symptoms mentioned above that suggest OSA, or a high score on the Epworth Sleepiness Scale, I may recommend certain tests. Many types of test can be done while you sleep; the most common ones include:
- Pulse Oximeter – Monitors the oxygen level in your blood by a probe clipped on to your finger.
- Polysomnography – This is the best but also the least available and most costly test that monitors various aspects of your sleep. It monitors the airflow through your nose, your chest movement, the electrical activity of your brain, snoring volume, blood oxygen saturation, and a video of your sleep. You may be asked to spend a night in the sleep lab for these tests to be done.
- I may also suggest other tests to exclude other causes of your sleepiness. For example, a blood test can check for an underactive thyroid gland or overactive pituitary gland.
Clinical examination
If you are bothered by significant snoring or have had tests showing OSA, a physical examination is carried out to see the site that is obstructing your airway. This includes an examination of your nose, throat, and voice box, most commonly by a bendy camera that is passed through one of your nostrils (flexible naso-laryngoscope). This is usually done in the clinic while you are awake.
What are the non-surgical treatment options?
Before having any operation, it is advisable to consider the following treatment options as the majority of OSA patients will benefit/get cured by these:
Changes to your lifestyle and habits
- This is the first step, and you may find a significant benefit from making the following changes:
- Losing some weight if you are overweight or obese
- Not drinking alcohol for 4-6 hours before going to bed
- Not using sedative drugs
- Stopping smoking if you are a smoker
- Sleeping on your side
- Keeping props under the head end of your bed to elevate it and by using extra pillows
Continuous positive airway pressure (CPAP)
This is the most effective non-surgical treatment for OSA and should be tried before considering an operation or if the changes mentioned above do not work or are not possible. CPAP involves wearing a mask when you sleep that is connected to an electrical machine that pumps room air into your nose at a slight pressure. The air pressure keeps the throat open when you are breathing at night, and so prevents the blockage of airflow. If CPAP works, then snoring is reduced or stopped, and there is an immediate improvement in sleep. Lifelong treatment is needed. Sometimes you can have problems with throat irritation or dryness, or bleeding inside your nose. We can treat these problems with newer CPAP machines that tend to have a humidifier fitted. Some people find the device cumbersome to wear at night. Due to these problems, around 40% to 50% of OSA patients fail to use CPAP for long.
Mandibular advancement devices
These are devices that you can wear inside your mouth when you sleep. They work by pulling the mandible forward a little so that your throat may not narrow as much in the night. These devices look a bit like gum shields that sports-people wear. To get the best results, you should get one tailor-made to the shape of your teeth and gums and properly fitted by a dentist.
What are the surgical options for treating snoring/OSA?
The operation aims to increase the airflow into your airway. The correct surgery for you would depend upon where your obstruction is and to what degree. As mentioned above, an accurate evaluation is critical to decide this so that the correct surgery is carried out for you
Tonsillectomy +/- Adenoidectomy
This is most commonly done in children with significant snoring or OSAS as relative large size of these structures is the most typical cause in that age group. Occasionally, adults have enlarged tonsils and will benefit from their removal.
Nose surgery
It is rare for your nose to be the cause of obstruction. If it is, an operation to straighten the nose, the septum inside or to widen the inside can be done. This can also be very useful if a blockage in your nose is making it difficult for you to use the CPAP machine.
Palatal Z plasty / modified uvulopalatopharyngoplasty (UVPP)
This is a procedure used to remove excess tissue in the throat to widen and allow air to move through the throat more easily when you breathe, reducing snoring. The tissues removed may include:
- The small finger-shaped piece of tissue (uvula) that hangs down from the back of the roof of the mouth into the throat
- Part of the roof of the mouth (soft palate)
- Enlarged throat tissue, tonsils, and adenoids
What to expect after UVPP
It takes about three weeks to recover from surgery. It can be quite painful, and it may be very difficult to swallow during this time. It is usual to notice small amount in blood in your throat or sputum while the wound heals itself. During the healing period, you may find yourself choking, especially when you drink thin fluid. You are likely to notice an improvement at about 3-4 weeks after the operation.
How successful is UVPP?
The success of UVPP is dependent on proper patient selection based on good examination by an experienced clinician. In carefully selected patients, it can cure snoring in 80% of those who have had this surgery.
What are the risks / potential complications of UVPP?
Like any other surgery, UVPP has some possible known complications, including:
- Swelling, infection, and bleeding
- Pain and trouble swallowing
- Drainage of secretions into the nose and a nasal quality to the voice
- Speech may be affected by this surgery
- Narrowing of the airway in the nose and throat
- Recurrence of snoring or OSA after a year or two
The last three complications mentioned above are relatively common with old-fashioned UVPP. However, the modified UVPP I offer has tremendously reduced these risks. I practice this modified technique of UVPP (Z-Palatoplasty), and I have found a very high satisfaction and success rate in my patients. Procedures for the roof of your mouth (palate) In some patients, surgery for the roof of the mouth is required as that is the main site of obstruction. The choice of procedure depends on the degree of obstruction related to how much excess tissue you have. Naturally, a precise diagnosis is crucial for successful treatment. By themselves, they are more useful for snoring but can be useful if done with one of the procedures mentioned above if you have sleep apnoea.
Coblation for Soft Palate and/Tongue
What causes snoring?
Snoring results from the vibration of throat tissue due to airflow. Usually, this occurs due to excessive volume and laxity of the soft palate /uvula and the back end of the tongue (lingual tonsil/base of the tongue).
During the assessment, I will perform an endoscopy to evaluate the exact site/s of actual narrowing. If this confirms that the narrow throat region leading to snoring is the palate and/or tongue base, your snoring is likely to improve/resolve by removal of excessive tissue and/or stiffening of the palate to reduce the narrowing and movement.
Coblation treatment for snoring?
Coblation is my preferred technique to stiffen or/and remove excess tissue from your soft palate and uvula. This is usually done under general anesthesia and takes 20 – 30 minutes. You are ready to go home after 4 hours.
The actual procedure involves removing the uvula (the dangling bit in the center of the palate), channelling under the surface of the palate and activating the instrument to remove and shrink tissue to reduce the size of the soft palate.
Recovery
Sleep with your head elevated for the first few days/nights.
It is common to experience some pain and throat swelling. Sucking on ice chips, gargling with aspirin solution (if not allergic) and taking Paracetamol/Ibuprofen can help relieve pain and swelling.
Similarly, you may notice some difficulty in swallowing or speaking for the first few days – all of these side effects will settle down within a week.
You will notice an improvement in 3-4 weeks after the procedure.
Palatal Z Plasty /Modified UVPP
Palatal Z plasty/modified UVPP treatment
If the amount of tissue in soft palate is excessive, stiffening procedures with coblation is not adequate. In such cases, you will require removal of the excess soft palate and tonsil area tissue. This will create extra space at the back of your nose and throat to breathe better while asleep.
Z plasty is a refined mechanism to achieve this and provides a better outcome and fewer problems compared to the traditional surgery (you may know the conventional operation as UVPP).
How?
This procedure is done under general anesthetic, i.e., while you are asleep. It involves strategic repositioning of the throat tissue with minimal removal to create more space behind your palate. This is done through your mouth with no visible scar and usually takes 30 – 45 minutes.
I usually combine this procedure with coblation, which involves shrinkage of the base of the tongue.
You will experience pain comparable to tonsillectomy, and this can take up to two weeks to resolve. During this period you will be given (in liquid form) pain killers, antibiotics and steroids and will have to rely on liquid or semisolid soft diet. Most patients are back to normal diet and swallowing in two to three weeks. However, for the first couple of months, you may experience fluid going up your nose from the throat, particularly if swallowed quickly.
You must schedule at least two weeks off from work to recover after this surgery.
You will notice an improvement in breathing and snoring after the swelling settles down, usually in 2-3 weeks.
Recovery
Sleep with your head elevated for the first few days/nights.
You will experience significant pain and throat swelling. Sucking on ice chips, gargling with aspirin solution (if not allergic) and taking Paracetamol/Ibuprofen can help relieve pain and swelling.
Similarly, you may notice some difficulty in swallowing or speaking for the first few days – all of these side effects should settle down within 2-3 weeks.
You will notice an improvement in 3-4 weeks after the procedure.
About ENT services
NHS – Functional Endoscopic Sinus Surgery
Provides an entire overview of the procedure. Click here for more information.
NHS – Tympanoplasty
Great advice for potential patients who are considering ear drum repair. Click here for more information.
NHS – Insertion of grommets
Goes over the risks, as well as the overall process of receiving ear grommets. Click here for more information.
NHS – Mastoidectomy
An NHS guide and overview of the treatment. Click here for more information.
Tinnitus.org – Balance and tinnitus
An overview of both the symptoms and treatments possible for balance and tinnitus. Click here for more information.
Cancer.gov – Parathyroid Cancer Treatment
A government website that gives a great amount of information on the cancer and treatment. Click here for more information.
NHS – Tonsillectomy
An overview of the symptoms and treatment. Click here for more information.
Consultation
We offer a free initial phone consultation with our specialist team. For the next step, we invite you to an in-person or online consultation with Mr Supriya. Consultations are £100 with Mr Supriya and are deductible from any booked surgery. This fee includes follow-up consultations.
Patient Stories
It’s embarrassing looking tired at work, and social events aren’t so fun when your confidence and self-esteem are lacking. You’ve neglected yourself and feel inadequate compared to all the beautiful people around you. You deserve some self-love.
Take your first step and step into a more beautiful you!
Meet Mr Supriya - The Best
Choice for Snoring Treatment

Meet Mr Mrinal Supriya | Facial Cosmetic Surgeon
FRCS (OTOL-HNS), MRCS Ed,
DO-HNS, MS in ENT, MBBS
Mr Mrinal Supriya is the Divisional Director of Surgery. He is highly experienced Head and Neck Surgeon, specialising in facial cosmetic surgery. He is Chief of Surgery Division (2024) and was the Clinical Director for head and neck surgery at Northampton General Hospital.
He leads complex ENT and head and neck services, including facial aesthetics & reconstruction and robotic surgery. Mr Supriya trained globally, including in the UK, Australia and the USA and worked with renowned experts like Dr Andrew Jacono. He is certified by The Royal College of Surgeons to provide facial cosmetic surgery in the UK.
Why Choose British Face Clinic for
Your Snoring Treatment?
- Focus on natural-looking outcomes and high patient satisfaction
- Benefit from Mr Supriya’s international experience
- Advanced surgical services led by Mr Supriya at a prominent NHS hospital
- Expertise in training Oxford Deanery Trainee Surgeons
- Address both cosmetic and medical issues with comprehensive care
- Exceptionally low revision rates
- Best possible support before, during and after surgery with dedicated team access
How to schedule a consultation
To schedule a consultation to discuss snoring treatment, you can either call us on 07590817036, book online via our website, schedule a video consultation or visit us at one of our clinics in London, Milton Keynes, or Northampton.
What to Expect During
Your Consultation
Welcome Message from Nidhi,
Director at British Face Clinic
During your full medical consultation, we’ll discuss:
- Your surgical goals
- Medical conditions, drug allergies and medical treatments
- Current medications, vitamins, supplements, alcohol, tobacco and drug use
- Previous surgeries
Our surgeon will:
- Evaluate your general health and risk factors
- Take photographs
- Discuss your surgical options
- Recommend a treatment course
- Discuss likely outcomes and potential complications
- Preview your surgical outcome with Crisalix 3D technology (for selected procedures)
- Discuss the surgery cost and payment options
Accessible Payment
Plans Now Available
We make your procedure more accessible by offering flexible payment plans with 0% interest for the first 12 months!
It takes less than a minute to fill in the form and receive a response. Snoring treatment has never been so accessible!
0% financing available

Change Your Life Today
Your freedom from snoring is just a free phone consultation away.
Contact us to learn how we can help you.
Our Locations
- London City
The Wellington Hospital, 15 – 17 Lodge Road
London NW8 7JA
- London City
98 Harley Street
London, W1G 7HZ
- Milton Keynes
Athena Surgical Centre
16 Davy Avenue, Knowlhill
Milton Keynes, MK5 8PL
- Northampton
The Three Shires Hospital
The Avenue
Northampton. NN1 5DR
London City
The Wellington Hospital
15 – 17 Lodge Road
London NW8 7JA
London City
98 Harley Street
London, W1G 7HZ
Milton Keynes
Athena Surgical Centre
16 Davy Avenue, Knowlhill
Milton Keynes, MK5 8PL
Northampton
The Three Shires Hospital
The Avenue
Northampton. NN1 5DR